Healthcare, biology and medicine has, for the last 3 centuries, been dominated by a model of understanding and teaching based on relatively simple, linear, hierarchical relationships and organ-based disciplines. It is now clear that hospitals and health care are more accurately described in terms of being complex adaptive systems.
What is this distinction and what does it mean for doctors?
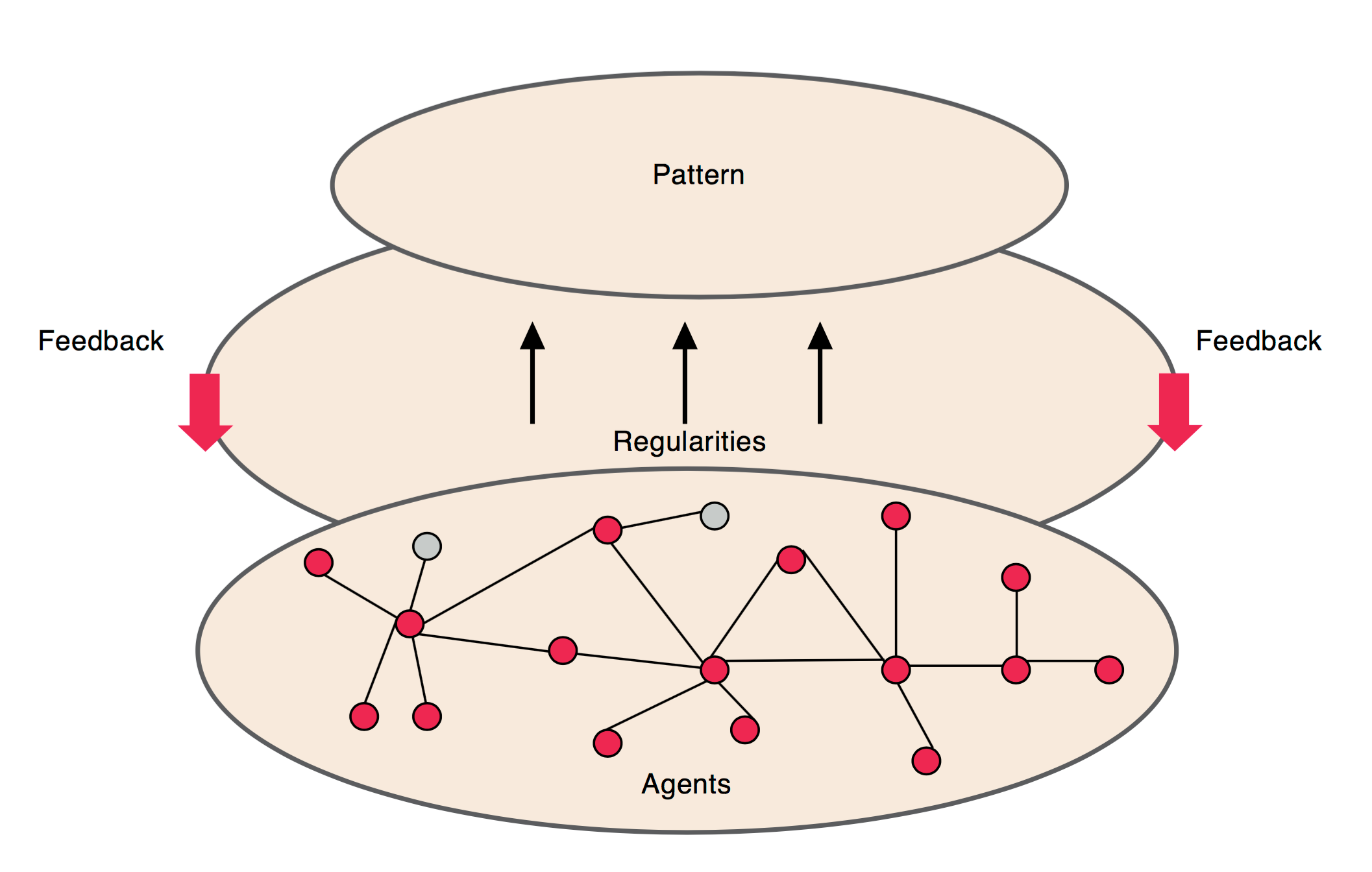
Complexity theory is based on relationships, emerging patterns and iterations. In complex adaptive systems, the agents within the system interact and connect with one another in unpredictable ways. All of the interactions within the system begin to form emerging patterns, which in turn feed back to the system and further influence the interactions of the agents.
The properties of these systems include:
- a large number of elements which interact dynamically
- any element of the system is affected by and affects other systems
- non-linear interactions, so small changes can have large effects
- a constant flow of energy to maintain organisation
- a history, whereby the past helps to shape present behaviour
- elements of the system are not aware of the behaviour of the system as a whole, and respond only to what is known or available locally
Simple representation of the components of a complex adaptive system (The Health Foundation, 2010)
Individual workers in one area of the system have a unpredictable effects on other areas of the organisation. Hospital managers may institute linear hierarchical change in an attempt to meet specific (often political) goals, but clinicians do not behave predictably. Without even acknowledging their own presence in an adaptive system, new processes on the floor are developed and tested, some discarded and others adopted. These intelligent micro-adaptations are frequently directed at keeping patients safe, when unexpected change interrupts established processes that are working well.
Clinicians have to be aware of the complexity of the system in which we work. We must expect unpredictability, respect the autonomy of individuals we work with and be flexible in responding to creativity, emerging patterns and opportunities in our workplace.
We all need to understand that medical practice is a complex adaptive system and be open to working in ways that achieve the best outcomes within that context.
Healthcare professionals in....
Traditional systems
Are controlling, mechanistic
Repeat the past
Are 'in charge'
Are autonomous
Are self-preserving
Resist change, bury contradictions
Are disengaged, nothing changes
Value position & structures
Hold formal position
Set rules
Make decisions
Are knowers
Complex adaptive systems
Are open, responsive, catalytic
Offer alternatives
Are collaborative
Are connected
Are adaptable
Acknowledge paradoxes
Are engaged, continuously emerging
Value persons
Are shifting as processes unfold
Prune rules
Help others
Are listeners
(from: Applying complexity science to health and healthcare)
A physician who acts within the spirit of a complex adaptive system views the patient as a human organism, not an indication for a procedure; understands the patient is embedded in a variety of systems—physiological, family, political, and social—that continuously recalibrate themselves; and appreciates that small interventions at the correct leverage points can have large results.
— Jessica Haupt, Plexus Institute.
Tools and approaches that might work well with simple problems will fail and disrupt when applied to complex ones. We must teach our junior doctors and medical students about the importance of skills in relationship and trust building, listening, empathy, how to respond to healthcare complexity and the importance of organisational learning.
These are the skill sets that will ensure a productive, happy career and result in long-lasting benefit for our patients and their families.
Further reading
People at the centre of complex adaptive health systems reform. MJA 2010 (PDF)
Applying complexity science to health and healthcare. Plexus Institute 2003 (PDF)